by Vignesh Subramanian, May 15, 2024
In 2023, the Centers for Disease Control and Prevention (CDC) published up-to-date data on suicide rates among American youth that stunned public health and medical professionals nationwide. The federal report, issued in June, found that the overall suicide rate among U.S. youth ages 10 to 24 had surged 62% over the prior two decades (2001-2021), after decades of prior decline (Curtin & Garnett, 2023). On average, 11 young Americans died by suicide out of every 100,000 each year during this period; for children ages 10-14, the suicide rate had tripled from 2007-2018 (from 0.9 to 2.9 people per 100,000); for adolescents ages 15-19, it rose 57% from 2009-2017 (from 7.5 to 11.8 people per 100,000); and for young adults ages 20-24, it rose 63% over the entire period (from 11.9 people in 2001 to 19.4 in 2021 per 100,000). The findings painted a stark picture of a nation in the throes of a full-fledged crisis, with millions of its young people suffering in silence and thousands compelled by circumstance to take their own lives.
Yet this grim milestone was seen by many as preceded by years of warning signs. Well before the COVID-19 pandemic, CDC reports noted that suicide rates among U.S. youth ages 10-24 had jumped 57.4% from 2007-2018 (rising from less than 7 deaths per 100,000 to nearly 11), with even such states as New York, New Jersey, and Massachusetts – widely viewed as having strong safety nets for at-risk youth – seeing increases in youth suicide rates ranging from 40% to 60% over that single decade (Curtin, 2020). The issue notably remained pervasive for young Americans of all ages. Between 2007 and 2019, the suicide rate among pre-teens ages 8 to 12 surged a disturbing 166% (Penfold, 2021), with 8.4% of children as young as nine and ten years old reporting suicidal thoughts and 1.3% even making attempts (Janiri et al., 2020). From 2018-2019, 18.8% of adolescents ages 12-17 seriously considered attempting suicide, with 15.7% making a suicide plan, 8.9% attempting suicide at least once, and 2.5% making an attempt that required medical treatment (Ivey-Stephenson et al., 2020), corresponding to around 1.24 million medically attended suicide attempts by American teenagers nationwide. This data came on the heels of separate studies finding that suicide rates more than doubled in the preceding decade (from approximately 2 deaths per 100,000 people in 2008 to 5 per 100,000 in 2018) for adolescents as young as thirteen and fourteen years old (Levine et al., 2023). And since 2019, emerging American adults ages 18-25 have demonstrated the highest prevalence of both serious suicidal thoughts (11.8% in 2019, rising to 13.6% by 2022) and suicide attempts made (1.8% in 2019, rising to 2.7% by 2021 before dropping to 2.1% by 2022) among adults across all age groups (National Institute of Mental Health, 2024; Richesson et al., 2022; Keating & Rudd-Arieta, 2021).
In 2023, the Centers for Disease Control and Prevention (CDC) published up-to-date data on suicide rates among American youth that stunned public health and medical professionals nationwide. The federal report, issued in June, found that the overall suicide rate among U.S. youth ages 10 to 24 had surged 62% over the prior two decades (2001-2021), after decades of prior decline (Curtin & Garnett, 2023). On average, 11 young Americans died by suicide out of every 100,000 each year during this period; for children ages 10-14, the suicide rate had tripled from 2007-2018 (from 0.9 to 2.9 people per 100,000); for adolescents ages 15-19, it rose 57% from 2009-2017 (from 7.5 to 11.8 people per 100,000); and for young adults ages 20-24, it rose 63% over the entire period (from 11.9 people in 2001 to 19.4 in 2021 per 100,000). The findings painted a stark picture of a nation in the throes of a full-fledged crisis, with millions of its young people suffering in silence and thousands compelled by circumstance to take their own lives.
Yet this grim milestone was seen by many as preceded by years of warning signs. Well before the COVID-19 pandemic, CDC reports noted that suicide rates among U.S. youth ages 10-24 had jumped 57.4% from 2007-2018 (rising from less than 7 deaths per 100,000 to nearly 11), with even such states as New York, New Jersey, and Massachusetts – widely viewed as having strong safety nets for at-risk youth – seeing increases in youth suicide rates ranging from 40% to 60% over that single decade (Curtin, 2020). The issue notably remained pervasive for young Americans of all ages. Between 2007 and 2019, the suicide rate among pre-teens ages 8 to 12 surged a disturbing 166% (Penfold, 2021), with 8.4% of children as young as nine and ten years old reporting suicidal thoughts and 1.3% even making attempts (Janiri et al., 2020). From 2018-2019, 18.8% of adolescents ages 12-17 seriously considered attempting suicide, with 15.7% making a suicide plan, 8.9% attempting suicide at least once, and 2.5% making an attempt that required medical treatment (Ivey-Stephenson et al., 2020), corresponding to around 1.24 million medically attended suicide attempts by American teenagers nationwide. This data came on the heels of separate studies finding that suicide rates more than doubled in the preceding decade (from approximately 2 deaths per 100,000 people in 2008 to 5 per 100,000 in 2018) for adolescents as young as thirteen and fourteen years old (Levine et al., 2023). And since 2019, emerging American adults ages 18-25 have demonstrated the highest prevalence of both serious suicidal thoughts (11.8% in 2019, rising to 13.6% by 2022) and suicide attempts made (1.8% in 2019, rising to 2.7% by 2021 before dropping to 2.1% by 2022) among adults across all age groups (National Institute of Mental Health, 2024; Richesson et al., 2022; Keating & Rudd-Arieta, 2021).
Surges in suicidal ideation and attempts among young Americans subsequently contributed to sharp increases in long-running trends of associated emergency department (ED) visits and hospitalizations. From 2011-2020, pediatric ED visits by children, adolescents, and young adults ages 6-24 nearly doubled nationwide (from 4.8 million visits, or 7.7% of all pediatric ED visits, to 7.5 million, or 13.1% of all visits), even as the overall number of pediatric ED visits for all causes decreased (Bommersbach et al., 2023). This spike in visits included a five-fold increase in the number of pediatric ED visits for suicide-related symptoms (from 0.9% of all visits in 2011 to 4.2% in 2020), which now make up an average of 5% of all visits by this age group. This alarming trend has been substantiated by other large national studies examining related healthcare data. Analyses of insurance claims for 24.5 million youths ages 1-21 found that mental health-related inpatient hospital admissions surged 61% among this population between 2016-2021, alongside a 45% increase in mental health-related ED visits and a 74% increase in ED visits for suicidal ideation, attempts, and self-harm by 2022, with the increases being most pronounced for adolescents and young adults (Clarify Health Institute, 2022; Clarify Health Institute, 2023). A review of 4.8 million pediatric hospitalizations from 2009-2019 at U.S. acute care hospitals revealed that a diagnosis of suicide or self-injury made up 64% of all mental health-related hospitalizations (Arakelyan et al., 2023). Other studies have found that all mental-related pediatric ED visits among youths ages 3-17 rose 8% annually from October 2015 to February 2020 (compared to an average increase of just 1.5% for visits for other reasons) (Cushing et al., 2022), with 13% of all patients revisiting within 6 months, and that from 2019-2020 – the last full year before the pandemic – the overall number of behavioral health cases for youth under 18 increased 30%, with pediatric ED cases of suicide attempts and self-injury in particular having jumped 50% (Children’s Hospital Association, 2023).
It was this already escalating crisis that proceeded to become severely exacerbated by the pandemic: in 2021, the first full year of the pandemic in the United States, the national suicide rate among youths 10-24 years old returned to 2018 highs after two years of moderate declines (Stone et al, 2023; Curtin et al., 2022). The stressful impacts of the period were acutely felt by young Americans of varied educational levels. The CDC found that 22% of U.S. high school students – including roughly a third (30%) of female students (Gaylor et al., 2023) – had seriously considered suicide the previous year, with 18% making a plan and 10% attempting at least once (drastically up from 16%, 13%, and 8% a decade prior, respectively) (CDC, 2023b). Separate reports also noted that three months into the pandemic, roughly a quarter (25.5%) of young people ages 18-24 – the largest age demographic on college campuses – had seriously considered suicide in the prior 30 days (Czeisler et al., 2020), and a Healthy Minds Survey found that 15% of U.S. college students surveyed during the 2021-2022 school year had seriously considered suicide, the highest rate in the survey’s 15-year history (Eisenberg et al., 2023). The CDC further found that beginning in April 2020 – shortly after the start of the pandemic in the United States – and proceeding through October of that same year, the proportion of mental health emergency-related visits among all pediatric ED visits surged 24% for children ages 5 to 11 and 31% for those ages 12 to 17 relative to 2019 levels (Leeb et al., 2020). In the second full year of the pandemic (from March 2021 to February 2022), pediatric mental health-related ED visits for youths ages 5-17 collectively jumped another 7%; the percentage of their ED visits resulting in psychiatric inpatient admission rose 8%; and the mean length of their stay increased 4%, with youth in both years of the pandemic more likely to spend two or more nights experiencing prolonged boarding (Overhage et al., 2023).
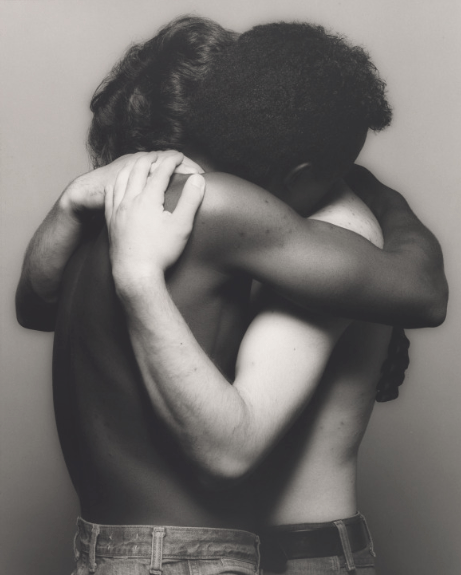
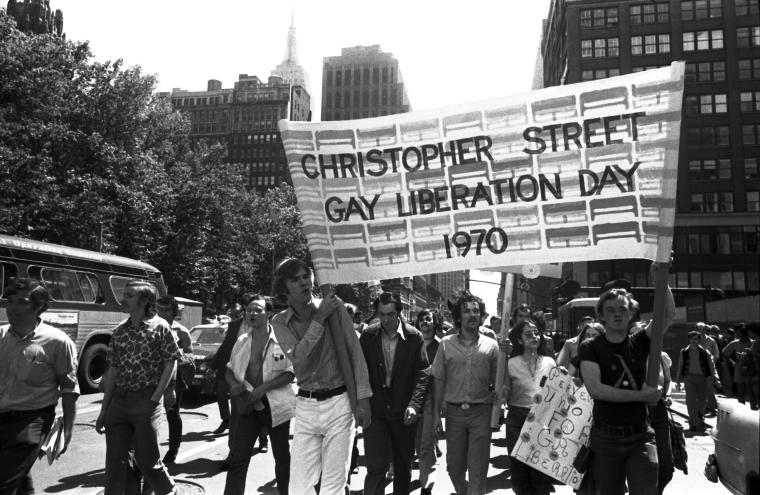
Overall, amid the pandemic, U.S. youth and young adults ages 10-24 began to represent 15% of all suicides nationally, and demonstrated exorbitantly high rates of ED visits for mental health emergencies and self-harm in particular, with 354.4 such visits per 100,000 members of this population in 2020 (compared to 128.9 visits per 100,000 people for middle-aged adults) (CDC, 2023a). Adolescent girls were noted to be at particularly high risk, with the proportion of ED visits for suicide attempts among those ages 12-17 jumping 50.6% from February-March 2019 to February-March 2021 (compared to just a 3.7% increase for boys and young men of the same ages) (Yard et al., 2021). Girls and young women ages 10-24 overall demonstrated a 43.6% increase in visits for suicidal ideation over the past two decades (Overhage et al., 2023), as well as an associated ED visit rate in 2021 measuring roughly double that of boys and young men (though the latter themselves consistently report some of the largest increases in suicide rates, including an 8% increase among those ages 15-24 in the same year) (CDC, 2023a; Curtin et al., 2022). Even more stark disparities in suicide rates have been discovered among other marginalized groups – with over a quarter of LGBTQ+ youths reporting attempting suicide in 2021, a significantly higher rate than that of their peers (Jones et al., 2022); higher percentages of American Indian and Alaska Native (AI/AN) youths experiencing suicidality than any other race or ethnicity that same year; Latina adolescents consistently being twice as likely to attempt suicide than their peers of the same race (Ivey-Stephenson et al., 2020); Black youths experiencing the largest percentage increases in suicides among any racial group in recent years (Stone et al., 2023); and Asian American/Pacific Islander (AAPI) adolescents and young adults being the only racial group to have suicide rank as their leading cause of death (CDC, 2018) – that merit an entirely separate article beyond the limitations of this paper.
For several years, U.S. lawmakers have demonstrated a propensity to pin the blame for the country’s youth suicide crisis entirely on the pandemic – despite such claims not covering the full story (Warner & Zhang, 2022). It is clear that this crisis had already reached epidemic proportions by the time COVID-19 took hold in early 2020. Yet even if this myopic view of its origins is genuinely held by those in elected office, it has failed to translate into substantive policy reforms that might address the widespread and life-threatening struggles with mental health currently faced by millions of young Americans. Nearly two full years into the pandemic (in October 2021), the American Academy of Pediatrics (AAP), the American Academy of Child and Adolescent Psychiatry, and the Children’s Hospital Association joined together to issue the unprecedented declaration of a national state of emergency in children’s mental health (AAP et al., 2021). The declaration took into account “dramatic increases” in rates of pediatric suicidality and ED visits for mental health emergencies, and called upon “policymakers at all levels of government and advocates for children and adolescents to join us” in working to institute a series of reforms, including securing sustainable funding for mental health screenings, establishing suicide prevention programs and risk assessments in schools and primary care, and addressing acute care needs in hospital settings by expanding access to adequate numbers of beds, step-down programs from inpatient units, and short-stay stabilization units, among other measures (Hua et al., 2024). Less than two months later, the U.S. Surgeon General echoed these calls, issuing an advisory highlighting the scope of the youth mental health crisis and outlining recommendations for governments and private healthcare organizations to collaborate to support children’s emotional and social well-being (Office of the U.S. Surgeon General, 2021), and roughly a year later, the AAP and over 130 other healthcare organizations explicitly called upon the Biden administration to declare a federal national emergency in children’s mental health (AAP et al., 2022). Yet despite these high-profile calls to action, no comprehensive federal legislation has been passed to support crisis identification, prevention, and intervention services for youth in either community or hospital settings (Roubein & Beard, 2022), and President Biden has yet to declare a national emergency in youth mental health, neglecting an opportunity to mobilize the full leverage and resources of the federal government to address the crisis.
At the state and local levels, attempts to contend with the youth suicide crisis have hardly fared better. As of June 2023, while half of all U.S. states and D.C. have enacted laws over the past decade that uniformly require their K-12 schools and school districts to adopt suicide prevention and intervention policies and guidelines outlining how staff should respond to students exhibiting suicidal ideation, 25 states have still not done so, according to the American Foundation for Suicide Prevention (AFSP, 2023). Furthermore, while 13 states uniformly require K-12 school personnel to be annually trained in such prevention and intervention protocols, a plurality of states (24, plus D.C.) do not mandate such training to occur every year – raising the risk that recall of key protocols may be poor in an emergency – and another 13 states do not require training at all. 22 states also uniformly require schools to develop curricula for student education in either suicide awareness and prevention and/or mental health more generally, but a majority (28, plus D.C.) continue not to do so. Statewide policy is even less consistent at the collegiate level, with 22 states having enacted laws uniformly requiring colleges and universities to adopt various specified suicide prevention policies – ranging from printing hotline numbers on student ID cards and publicizing student mental health resource information to adopting institutional awareness programs or prevention and intervention strategies – while the majority of states (28, plus D.C.) lacked any laws establishing a uniform standard of preparedness for higher education institutions as of December 2022 (AFSP, 2022). The resulting patchwork of policies, fragmented across thousands of campuses and communities, fails to offer a comprehensive response to the nationwide youth suicide crisis that transcends their outskirts and borders. Meanwhile, conflicting guidelines on the ages at which youths are recommended to be screened early in childhood for suicide risk (the AAP recommends those ages 12 and up be universally screened annually, with those ages 8-11 screened when clinically indicated, while the U.S. Preventive Services Task Force argues there is insufficient evidence to justify screening any asymptomatic youths for suicide risk) continue to confuse localities and providers seeking to address the root causes of such ideation (Jenco, 2022). Hospitals and inpatient facilities are also becoming overwhelmed by surging numbers of suicidal young adults, adolescents, and increasingly younger-aged children who arrive in EDs already at their crisis point (Richtel & Flanagan, 2022), with no end to this epidemic in sight as of yet.
Today, suicide is the third leading cause of death among young Americans ages 15-24 and the second leading cause of death among those ages 10-14. The United States loses far more of its young people to suicide than any other developed nation each year, with the total number of lives lost representing a disproportionately large segment of its youth population (Doran & Kinchin, 2020). For every young person lost to suicide, roughly 1,000 others are estimated to be considering and struggling with the idea of attempting (National Alliance on Mental Illness, 2024) – but every one of these suicides is preventable. Despite having an abundance of options with which to act, the nation’s leaders have collectively and inexcusably allowed this crisis to spiral out of control, and in so doing, have left millions of vulnerable children, adolescents, and young adults at risk. We must act swiftly and decisively to change course, advancing reforms that will reshape national policy to confront these harsh clinical realities – and ultimately save lives.
Works Cited
- American Academy of Pediatrics, American Academy of Child and Adolescent Psychiatry, & Children’s Hospital Association. (2021). AAP-AACAP-CHA declaration of a national emergency in child and adolescent mental health. American Academy of Pediatrics. https://www.aap.org/en/advocacy/child-and-adolescent-healthy-mental-development/aap-aacap-cha-declaration-of-a-national-emergency-in-child-and-adolescent-mental-health/
- American Academy of Pediatrics, American Academy of Child and Adolescent Psychiatry, & Children’s Hospital Association. (2022). Health organizations urge the Biden administration to declare a federal national emergency in children’s mental health. American Academy of Pediatrics. https://www.aap.org/en/news-room/news-releases/aap/2022/health-organizations-urge-the-biden-administration-to-declare-a-federal-national-emergency-in-childrens-mental-health/
- American Foundation for Suicide Prevention. (2023). Policy priority: Suicide prevention in schools (K-12). American Foundation for Suicide Prevention Public Policy Office. https://www.datocms-assets.com/12810/1686164392-afsp-k-12-schools-issue-brief.pdf
- American Foundation for Suicide Prevention. (2022). Policy priority: Suicide prevention on university and college campuses. American Foundation for Suicide Prevention Public Policy Office. https://www.datocms-assets.com/12810/1677181582-afsp-colleges-universities-issue-brief.pdf
- Arakelyan, M., Freyleue, S., Avula, D., McLaren, J. L., O’Malley, A. J., & Leyenaar, J. K. (2023). Pediatric mental health hospitalizations at acute care hospitals in the US, 2009-2019. JAMA, 329(12), 1000-1011. DOI: 10.1001/jama.2023.1992
- Bommersbach, T. J., McKean, A. J., Olfson, M., & Rhee, T. G. (2023). National trends in mental health–related emergency department visits among youth, 2011-2020. JAMA, 329(17), 1469-1477. DOI: 10.1001/jama.2023.4809
- Centers for Disease Control and Prevention. (2018). LCWK1 – Deaths, percent of total deaths, and death rates for the 15 leading causes of death in 5-year age groups, by race and Hispanic origin, and sex: United States, 2017. Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System, 1-195. https://www.cdc.gov/nchs/data/dvs/lcwk/lcwk1_hr_2017-a.pdf
- Centers for Disease Control and Prevention. (2023a). Disparities in Suicide. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. https://www.cdc.gov/suicide/facts/disparities-in-suicide.html
- Centers for Disease Control and Prevention. (2023b). Youth Risk Behavior Survey data summary & trends report: 2011-2021. Centers for Disease Control and Prevention, Division of Adolescent and School Health. https://www.cdc.gov/healthyyouth/data/yrbs/pdf/YRBS_Data-Summary-Trends_Report2023_508.pdf
- Children’s Hospital Association. (2023). The latest pediatric mental health data. Children’s Hospital Association. https://www.childrenshospitals.org/news/childrens-hospitals-today/2023/04/the-latest-pediatric-mental-health-data
- Clarify Health Institute. (2022). The kids are not alright – Pediatric mental health care utilization from 2016-2021. Clarify Health. clarifyhealth.com/wp-content/uploads/2022/09/The-Clarify-Health-Institute-Research-Brief_The-Kids-Are-Not-Alright.pdf
- Clarify Health Institute. (2023). The kids are not alright – Mental health utilization among children and young adults: 2016-2022. Clarify Health. clarifyhealth.com/wp-content/uploads/2023/05/Clarify-Health-Institute-Research-Brief-The-Kids-Are-Not-Alright-2023.pdf
- Curtin, S.C. (2020). State suicide rates among adolescents and young adults aged 10–24: United States, 2000–2018. Centers for Disease Control and Prevention, National Vital Statistics Reports, 69(11), 1-10. https://www.cdc.gov/nchs/data/nvsr/nvsr69/nvsr-69-11-508.pdf
- Curtin, S .C. & Garnett, M. F. (2023). Suicide and homicide death rates among youth and young adults aged 10–24: United States, 2001–2021. Centers for Disease Control and Prevention, National Center for Health Statistics (471). DOI: 10.15620/cdc:128423
- Curtin, S. C., Garnett, M. F., & Ahmad, F. B. (2022). Provisional Numbers and Rates of Suicide by Month and Demographic Characteristics: United States, 2021. Centers for Disease Control and Prevention, National Vital Statistics Reports, (24), 1-7. https://www.cdc.gov/nchs/data/vsrr/vsrr024.pdf
- Cushing, A. M., Liberman, D. B., Pham, P. K., Michelson, K. A., Festekjian, A., Chang, T. P., & Chaudhari, P. P. (2022). Mental health revisits at US pediatric emergency departments. JAMA Pediatrics, 177(2), 168-176. DOI: 10.1001/jamapediatrics.2022.4885
- Czeisler, M. E., Lane, R. I., Petrosky, E., Wiley, J. F., Christensen, A., Njai, R., Weaver, M. D., Robbins, R., Facer-Childs, E. R., Barger, L. K., Czeisler, C. A., Howard, M. E., & Rajaratnam, S. M. W. (2020). Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. Centers for Disease Control and Prevention, Morbidity and Mortality Weekly Report, 69(32), 1049-1057. DOI: 10.15585/mmwr.mm6932a1
- Doran, C. M. & Kinchin, I. (2020). Economic and epidemiological impact of youth suicide in countries with the highest human development index. PLOS One, 15(5). DOI: 10.1371/journal.pone.0232940
- Eisenberg, D., Lipson, S. K., Heinze, J., Zhou, S., Vyletel, B., Henry, H., Fucinari, J., Murphy, M., Voichoski, E., & Inscore, A. (2023). The Healthy Minds Study: 2021-2022 data report. Healthy Minds Network. https://healthymindsnetwork.org/wp-content/uploads/2023/08/HMS-National-Report-2021-22_full.pdf
- Gaylor, E. M., Krause, K. H., Welder, L. E., Cooper, A. C., Ashley, C., Mack, K. A., Crosby, A. E., Trinh, E., Ivey-Stephenson, A. Z., & Whittle, L. (2023). Suicidal thoughts and behaviors among high school students — Youth Risk Behavior Survey, United States, 2021. Centers for Disease Control and Prevention, Morbidity and Mortality Weekly Report, 72(1), 45-54. DOI: 10.15585/mmwr.su7201a6
- Hua, L. L., Lee, J., Rahmandar, M. H., Sigel, E. J., Committee on Adolescence, & Council on Injury, Violence, and Poison Prevention. (2024). Suicide and suicide risk in adolescents. Pediatrics, 153(1). DOI: 10.1542/peds.2023-064800
- Ivey-Stephenson, A. Z., Demissie, Z., Crosby, A. E., Stone, D. M., Gaylor, E., Wilkins, N., Lowry, R., & Brown, M. (2020). Suicidal ideation and behaviors among high school students — Youth Risk Behavior Survey, United States, 2019. Centers for Disease Control and Prevention, Morbidity and Mortality Weekly Report, 69(1), 47-55. DOI: 10.15585/mmwr.su6901a6
- Janiri, D., Doucet, G., Pompili, M., Sani, G., Luna, B., Brent, D., & Frangou, S. (2020). Risk and protective factors for childhood suicidality: a US population-based study. The Lancet Psychiatry, 7(4), 317-326. DOI: 10.1016/S2215-0366(20)30049-3
- Jenco, M. (2022). AAP urges suicide screening despite USPSTF call for more research. American Academy of Pediatrics News. https://publications.aap.org/aapnews/news/19948/AAP-urges-suicide-screening-despite-USPSTF-call
- Jones, S. E., Ethier, K. A., Hertz, M., DeGue, S., Le, V. D., Thornton, J., Lim, C., Dittus, P. J., & Geda, S. (2022). Mental health, suicidality, and connectedness among high school students during the COVID-19 pandemic — Adolescent behaviors and experiences survey, United States, January–June 2021. Centers for Disease Control and Prevention, Morbidity and Mortality Weekly Report, 71(3), 16-21. https://www.cdc.gov/mmwr/volumes/71/su/pdfs/su7103a1-a5-H.pdf
- Keating, S. R. & Rudd-Arieta, M. (2021). Emerging adults’ attitudes and beliefs about suicide and technology/social media. The Journal for Nurse Practitioners, 17(7), 833-839. DOI: 10.1016/j.nurpra.2021.04.010
- Leeb, R. T., Bitsko, R. H., Radhakrishnan, L., Martinez, P., Njai, R., & Holland, K. M. (2020). Mental health–related emergency department visits among children aged <18 years during the COVID-19 pandemic — United States, January 1–October 17, 2020. Centers for Disease Control and Prevention, Morbidity and Mortality Weekly Report, 69(45), 1675-1680. DOI: 10.15585/mmwr.mm6945a3
- Levine, R. S., Levine, E. M., Rubenstein, A., Muppala, V., Mejia, M. C., Gonzalez, S., Zoorob, R. J., Hennekens, C. H., & Wood, S. K. (2023). Continuing alarming increases in suicide in American youths: Clinical and research challenges. Annals of Pediatrics and Child Health. https://www.jscimedcentral.com/jounal-article-pdfd/Annals-of-Pediatrics-and-Child-Health/pediatrics-11-1301.pdf
- National Institute of Mental Health. (2024). Suicide. The National Institutes of Health. https://www.nimh.nih.gov/health/statistics/suicide
- National Alliance on Mental Illness (2024). What you need to know about youth suicide. NAMI. https://www.nami.org/Your-Journey/Kids-Teens-and-Young-Adults/What-You-Need-to-Know-About-Youth-Suicide
- Office of the U.S. Surgeon General. (2021). Protecting youth mental health: The U.S. Surgeon General’s advisory. U.S. Department of Health and Human Services, Office of the U.S. Surgeon General. https://www.hhs.gov/surgeongeneral/priorities/youth-mental-health/index.html
- Overhage, L., Hailu, R., Busch, A. B., Mehrotra, A., Michelson, K. A., & Huskamp, H. A. (2023). Trends in acute care use for mental health conditions among youth during the COVID-19 pandemic. JAMA Psychiatry, 80(9), 924-932. DOI: 10.1001/jamapsychiatry.2023.2195
- Penfold, R. (2021). Addressing the crisis of youth suicide in America. Kaiser Permanente Washington Health Research Institute. https://www.kpwashingtonresearch.org/news-and-events/blog/2021/addressing-crisis-youth-suicide-america
- Richesson, D., Magas, I., Brown, S., Hoenig, J. M., Cooper, P. M., Gyawali, S., Smith, T., & Yen, J. (2022). Key Substance Use and Mental Health Indicators in the United States: Results from the 2021 National Survey on Drug Use and Health. Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/sites/default/files/reports/rpt39443/2021NSDUHFFRRev010323.pdf
- Richtel, M. & Flanagan, A. (2022). Hundreds of suicidal teens sleep in emergency rooms. Every night. The New York Times. https://www.nytimes.com/2022/05/08/health/emergency-rooms-teen-mental-health.html
- Roubein, R. & Beard, M. (2022). Congress is working on legislation to address children’s mental health crisis. The Washington Post. www.washingtonpost.com/politics/2022/06/01/congress-is-working-legislation-address-children-mental-health-crisis/
- Stone, D. M., Mack, K. A., & Qualters, J. (2023). Notes from the field: Recent changes in suicide rates, by race and ethnicity and age group — United States, 2021. Centers for Disease Control and Prevention, Morbidity and Mortality Weekly Report, 72(6), 160-162. DOI: 10.15585/mmwr.mm7206a4
- Warner, J. & Zhang, J. (2022). ‘We have essentially turned a blind eye to our own children for decades’: Why we need to stop politicizing children’s mental health. The Washington Post Magazine. https://www.washingtonpost.com/magazine/2022/03/21/childrens-mental-health-crisis-politicization/
- Yard, E., Radhakrishnan, L., Ballesteros, M. F., Sheppard, M., Gates, A., Stein, Z., Hartnett, K., Kite-Powell, A., Rodgers, L., Adjemian, J., Ehlman, D. C., Holland, K., Idaikkadar, N., Ivey-Stephenson, A., Martinez, P., Law, R., & Stone, D. M. (2021). Emergency department visits for suspected suicide attempts among persons aged 12–25 years before and during the COVID-19 pandemic — United States, January 2019–May 2021. Centers for Disease Control and Prevention, Morbidity and Mortality Weekly Report, 70(24), 888-894. DOI: 10.15585/mmwr.mm7024e1